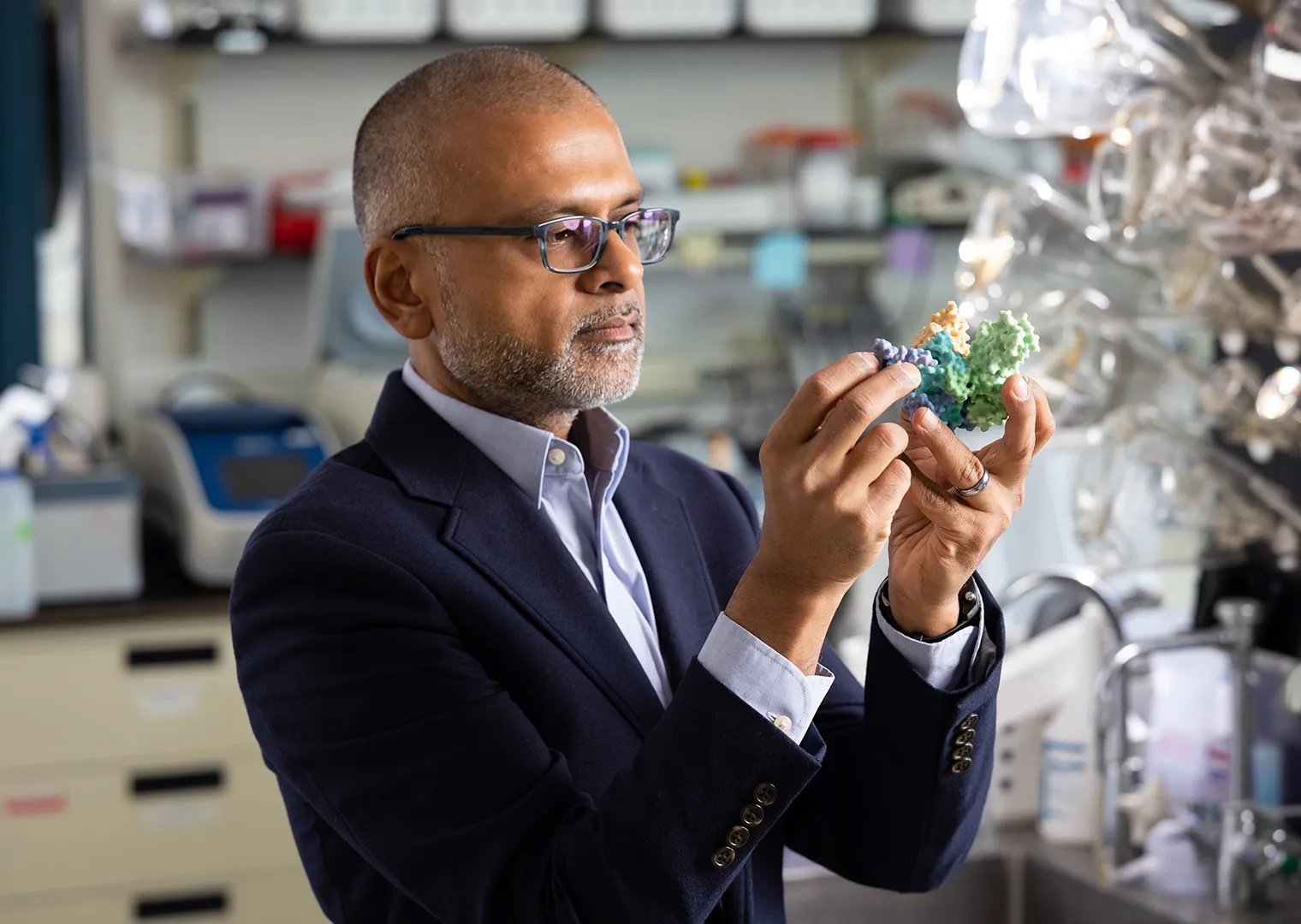
April 3, 2019—(BRONX, N.Y.)—The National Institute of Allergy and Infectious Diseases (NIAID) has awarded an international consortium led by Albert Einstein College of Medicine a five-year, $22 million grant to develop antibody-based therapies against four highly lethal viruses for which there are no approved vaccines or treatments.
The viruses are the tick-borne Crimean-Congo hemorrhagic fever virus (CCHFV) and three hantaviruses, which are spread by rodents: Andes virus (ANDV), Sin Nombre virus (SNV), and Puumala virus (PUUV). The NIAID has designated all but PUUV as Category A agents—emerging infectious diseases or pathogens that pose the highest risk to national security and public health.
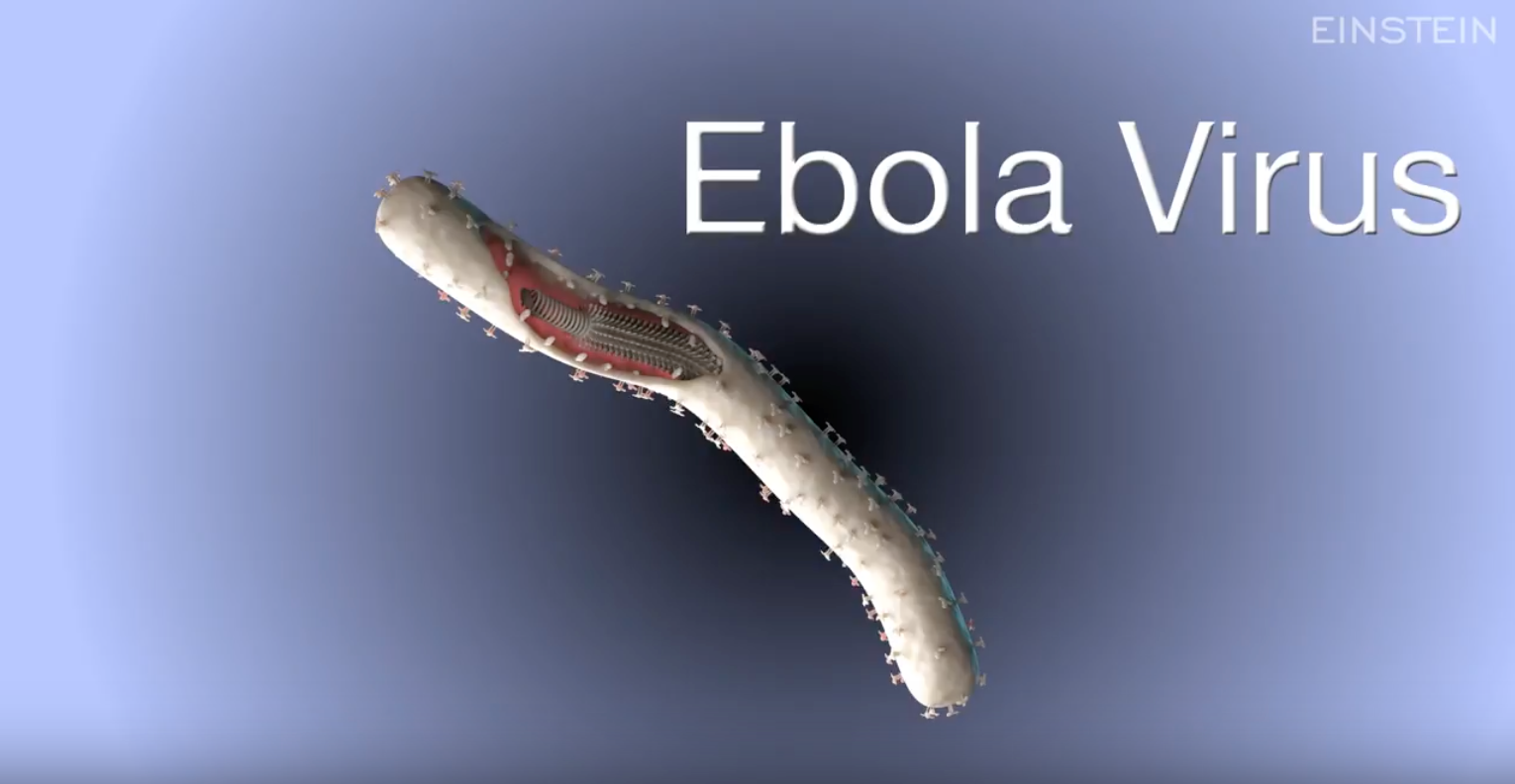
The project, called the Prometheus Center for Excellence in Translational Research (Prometheus), focuses on viruses that spread from animals to people. It builds on a 2017 study involving ebolaviruses, believed to spread to people from fruit bats or primates. In addition to Einstein, the participating institutions leading the project are the U.S. Army Medical Research Institute of Infectious Diseases (USAMRIID), Mapp Biopharmaceutical, Inc., The University of Texas at Austin, and Adimab, LLC, a biotech company.
Read more about Prometheus and watch a video about our team and work.